The State of Mental Health in a Post-Pandemic Society
In 1949, Congress declared May to be Mental Health Awareness Month, primarily because of the great number of WWII Veterans suffering from mental health issues. Over time, mental health awareness has sought to destigmatize and educate people about mental health, as well as provide education about the collective impact of mental health, not just on the individual, but on families, children, and society as a whole.
Over the past 70 years, we have seen an expansion of government programs to support people with mental health treatment and recovery, including the Affordable Care Act, which expanded insurance coverage for 30 million Americans, including an estimated 11 million people who now have access to previously unavailable mental health services. In 2008, the passing of the Mental Health Parity and Addiction Equity Act sought to increase the availability of mental health and substance use disorder treatment by requiring commercial insurance companies to provide the same access to these services as they do physical health services. However, while the Act calls for equitable access, enforcement is rare, and quality mental health services remain difficult to access through insurance. This is also true for Medicaid and Medicare, which have very poor rates of access to mental health services.
Even with improvements over the past decades in social programs, greater acceptance of therapy as an option for treatment, new developments in psychopharmacology to treat serious mental health disorders, the rates of mental health disorders are not improving. Treatment as usual for mental health, which typically includes diagnosis and medication, and sometimes counseling, isn’t turning the tide on what now, post-COVID-19, appears to be a mental health crisis in the U.S.
According to Mental Health America’s survey results in “The State of Mental Health in America 2023,” 21% of adults in the US experience a mental illness, or more than 50 million people. Of those adults, 55% receive no treatment. Forty-two percent of U.S. adults with a diagnosable condition reported in 2023 that they could not afford to access the treatment they needed. The rate of death by suicide has gone up 33% over the past 50 years; someone commits suicide every 40 seconds. And approximately 25 million adults in the United States have been on antidepressants for at least two years, which is a 60%increase in less than a decade.

Image description: A woman in a wheelchair sits facing a window with closed drapes. Her back is to the camera. Her hand is on her head as if she is distressed.
For people with disabilities, these statistics jump significantly. People with disabilities report frequent mental distress almost five more times than those without disabilities. In fact, Mental Illness is currently the leading cause of disability worldwide.
When the pandemic hit in 2020, mental health issues worsened. According to the CDC, from August 2020 to February 2021, the percentage of adults with recent symptoms of an anxiety or depressive disorder increased from 36.4% to 41.5%. Increased isolation, financial instability, challenges for online learning for students, and increased health concerns affected everyone, but it was much harder for people with disabilities. According to a 2022 survey by the American Association on Health & Disability, nearly 50% of people with disabilities dealt with new challenges accessing healthcare during the pandemic. As with many, they found their healthcare needs deprioritized over care for people with COVID-19 and had further difficulties accessing vaccinations due to inequities in the healthcare system. This was particularly challenging for people with disabilities who depend on health services or medications to remain independent, and likely worsened mental health across the board.
Financially, people with disabilities faced a steeper decline during the pandemic which contributed to a further decline in mental health. People with disabilities experienced higher rates of unemployment during COVID-19: 5.3% for people with disabilities compared to a 4.4% increase for people without disabilities. This is significant since only 17.9% of people with disabilities are in the workforce, typically earning less than median pay, therefore experiencing greater financial and emotional impact from the loss of employment.
Social isolation had the greatest impact on mental health for people during the pandemic. People with disabilities generally are at higher risk, so had to isolate further than those who aren’t. Approximately 50% of people claimed isolation as the number one cause of stress and deteriorating mental health during the pandemic.
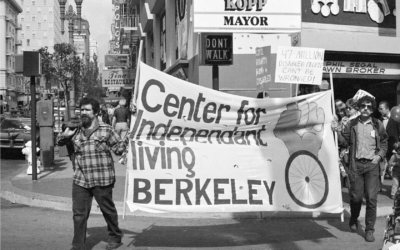
From In-Person to Online, Overnight
Before the pandemic, CPWD’s services were almost entirely offered in person. When COVID-19 hit, the organization had to make a massive shift and move everything online almost overnight. Recognizing that social isolation would be extremely detrimental, CPWD increased their Peer Support Groups from 3-4 times a month up to 1-2 per day. We reached out to all of our intake consumers to ensure that they were connected to necessary services and support. Over the course of the pandemic, we collaborated with vaccine clinics, medical services, and others to increase equitable access to health services, and found online ways to provide skills training, advocacy, and other independent living services. The sudden shift created a challenge for many people with disabilities. Beth Gustin was a Beyond Vision and mental health counselor for CPWD during that time.

Beth Gustin and her service dog Manolo. Image description: Beth Gustin is sitting outside on a flat bench. She is wearing a purple t-shirt, a floral scarf around her neck, and black pants. Her curly brown hair is chin-length. In front of her is sitting her black lab Manolo. He is wearing a harness with a protruding handle.
“COVID highlighted and exacerbated challenges that are inherent to people with disabilities, in particular people with vision loss,” Gustin explained. “Moving around in public, at the store, 6 feet apart, and so forth was so challenging that many avoided it, which led to increased isolation, and increased anxiety and/or depression.”
Even with an effective transition to online services, and an increase in services, the digital world presented new barriers for some people with disabilities. “Overall there was an increase in participation in these groups, but it took a bit. Everyone had to learn how to access those groups,” said Gustin. “Telehealth is great and has definitely decreased some access barriers. However, if you are in your late seventies or eighties, technology isn’t something you may be as familiar with. Not everyone can get online.”
For others, this new shift to the digital world was a blessing. Meira Merz, a consumer of CPWD and an Autistic person, explained how much this change helped her.
“I spent six years co-facilitating a support group. It is a safe space, and has been created with a lot of intentionality to be a safe space,” she said. “When Covid happened we went completely virtual. It was actually a lovely transition for a lot of the members. There were some people that didn’t like it because they needed in-person interaction. I personally prefer the virtual.”
Many people are not aware that several mental health disorders are considered disabilities. These disabilities are often hard to classify, and are considered the “invisible disabilities.” For this reason, many people don’t seek the help and support they need to live the best quality of life they are able to.
Maria Stepanyan, the Executive Director of CPWD, lives with a mental health disability.
“I have PTSD,” she explained, “which has brought a lot of depression and anxiety. At times it’s manageable, at times it’s not. And sometimes when you tell someone you have PTSD and you have depression and anxiety, sometimes it’s not taken as seriously because the hidden disabilities are often not understood.”
Seven percent of adults will have some form of PTSD in their lifetime. Fifteen million suffer from it in any given year.
It is important to seek professional help if you find yourself dealing with any type of mental health issues. People with many types of mental illnesses can qualify for disability benefits through the government. The Social Security Administration qualifies these mental health disorders for Social Security Disability Benefits:
- Affective disorders
- Anxiety Disorders
- Autism and related disorders
- Intellectual disabilities
- Organic Mental Disorders
- Personality disorders
- Schizophrenia, paranoia, and psychotic disorders
- Somatoform disorders
- Substance addiction

Peer Support Group: Image Description: At a Peer Support Group, four people sit looking forward. The woman on the far left sits in a wheelchair and reads from a book. She has short white hair. The woman next to her also sits in a wheelchair. She has a hand on her heart and has short dark hair and glasses. To her right is a young man in a wheelchair with dark hair and glasses. He is wearing a face mask and looking down. To his right is a young woman sitting in a chair. Her hands are in the prayer position at her heart. She has glasses and long blond hair.
Now as we are moving out of the pandemic, we are recognizing the need for a more balanced life that supports greater mental and emotional well-being. Remote work has afforded more work-life balance, yet at the same time, we are more chained to incessant technology – email and text, for example – than ever before. We are also faced with perpetual uncertainty regarding the economy, climate, increasing social violence, and other issues. One thing we can take away from COVID-19 is the need to increase our own level of self-care and self-awareness. Often, mild or moderate mental health issues can be managed through a healthy lifestyle and positive self-care before they become serious. How to do this harkens back to “Grandma’s wisdom:” Get enough sleep, eat healthily, don’t watch too much TV, avoid disturbing news stories, get outside, avoid drugs and alcohol, and most importantly, connect with others who you enjoy being with. For people with disabilities, CPWD’s Peer Support groups are a fantastic way to connect with others to share inspiration and strength.
If you feel like you need assistance finding support, CPWD may be able to guide you to resources and services that can help. You can reach out to one of our Independent Living Advisors here for information and referral on mental health support. Another good resource is the National Institute of Mental Health resources page where you can seek information and treatment. The National Center on Health, Physical Activity, and Disability (NCHPAD) have created a program called MENTOR (Mindfulness, Exercise, Nutrition to Optimize Resilience) specifically for people with a mobility disability. This eight-week program is free to anyone over 18 who has a disability and focuses on cultivating physical, mental, and emotional help by connecting people with a mental health counselor, fitness instructor, and dietician through virtual sessions. You can learn more and sign up for this program here. The Special Olympics created the Strong Minds Activity Guide for people with IDD to earn and follow activities to cultivate coping skills for stress and mental health.
Mental illness is devastating and can inhibit people from living healthy and independent lives. But it doesn’t have to. As we move forward into the future we must advocate not only for our own mental health but the mental health of society as a whole. We need further affordable and accessible mental health services and support lifestyles that prioritize mental health so we can begin to turn the tide and create a happier, healthier global community.